#SimBlog: Acute Heart Failure
““69-year-old female. Awoke short of breath 6 hours ago. No chest pain.””
Observations
A – Patent
B – Sats 88% (21%), RR 35
C – HR 135, BP 175/86
D – Alert
E – Pyrexial
Clinical Findings
Bilateral Crackles to the mid zones
Pitting Oedema
Raised JVP
Why We Simulated?
Difficulty in breathing is a frequent presentation to the ED, but can have a wide differential.
Acute heart failure is common with over 67,000 admissions in England and Wales per year (Dworzynski, Roberts, Dudman, Mant 2014) [1].
It is important to recognise the clinical features and the radiological appearance, as the differential for a patient with dyspnoea can be quite broad.
Appropriate management in the ED can make a significant difference to these patients. The current NICE guidelines do not recommend the use of opiates or the routine use of nitrites (IV nitrates are for use in specific circumstances and should warrant level 2 care).
It is therefore important to involve cardiology, outreach, or even critical care to support these patients on the wards. The NICE guidelines recommend that all patients admitted with heart failure should be managed by cardiology or have input from a Heart Failure Outreach team.
Learning Points
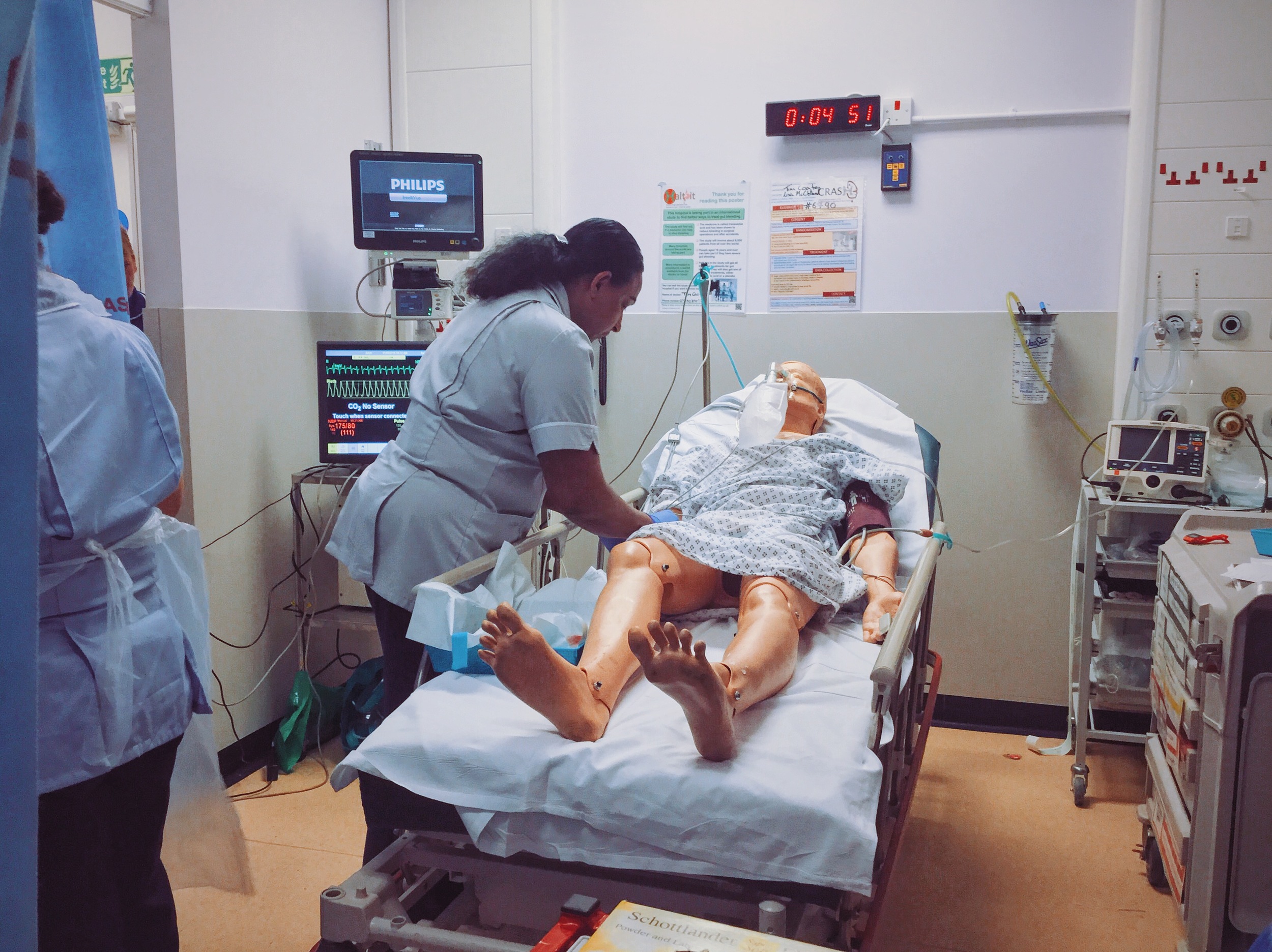
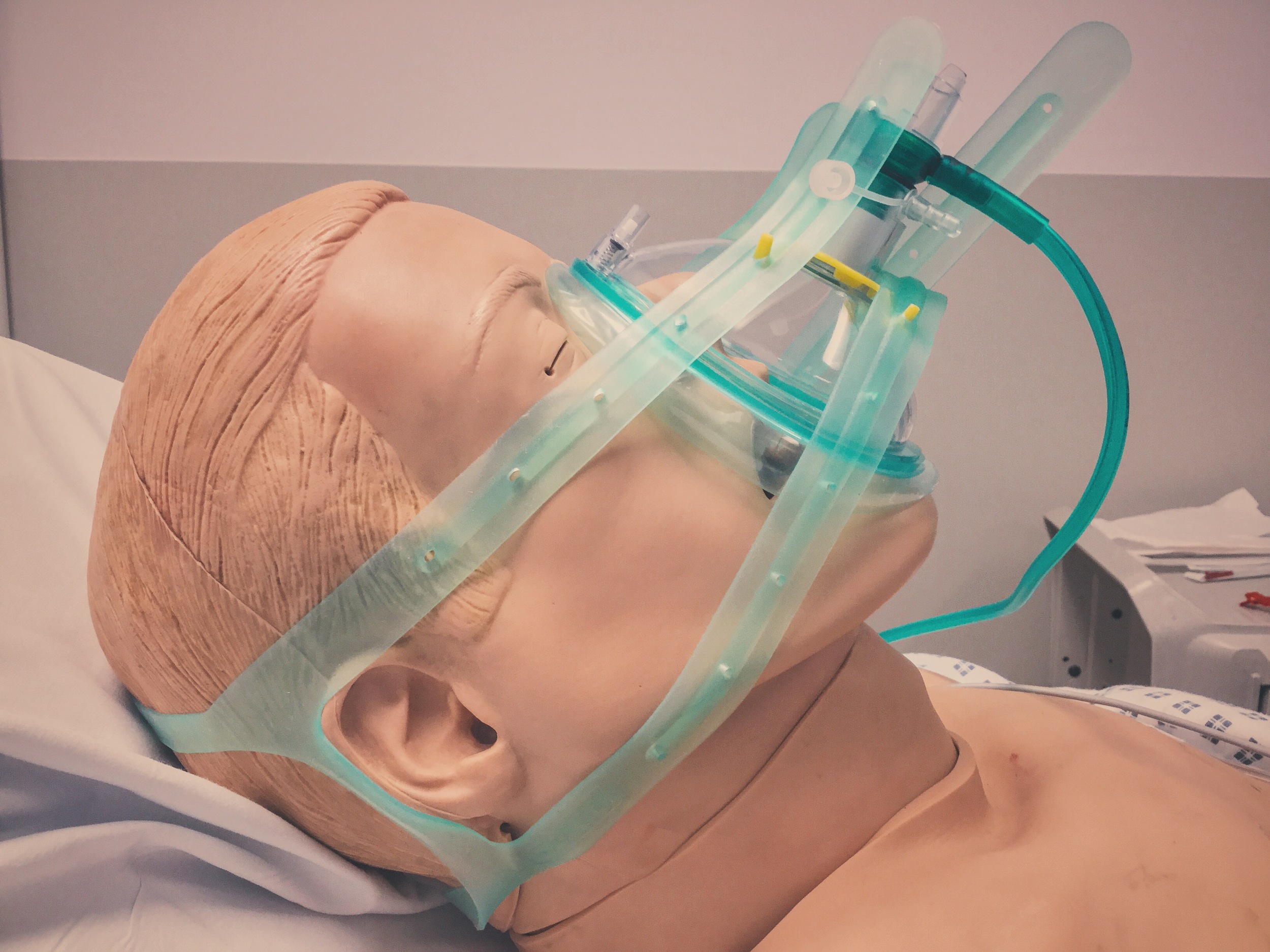
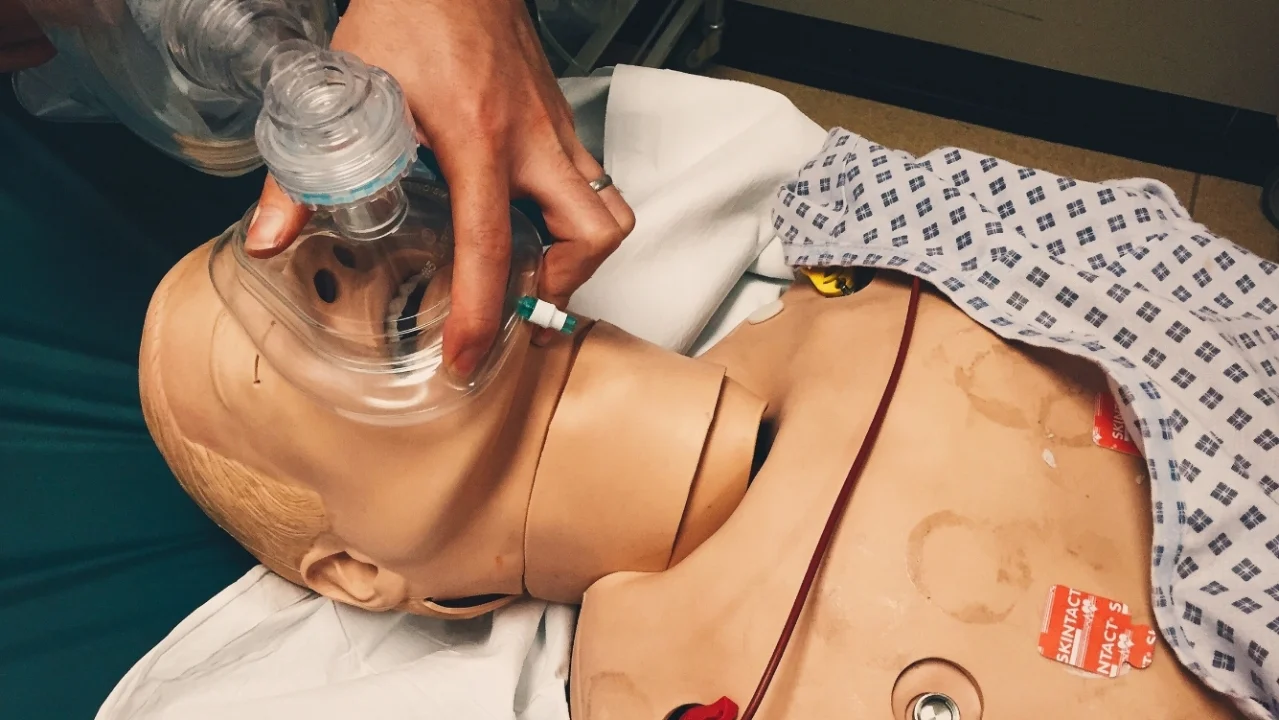
Indications for CPAP
Task overload and feedback
CPAP circuit location
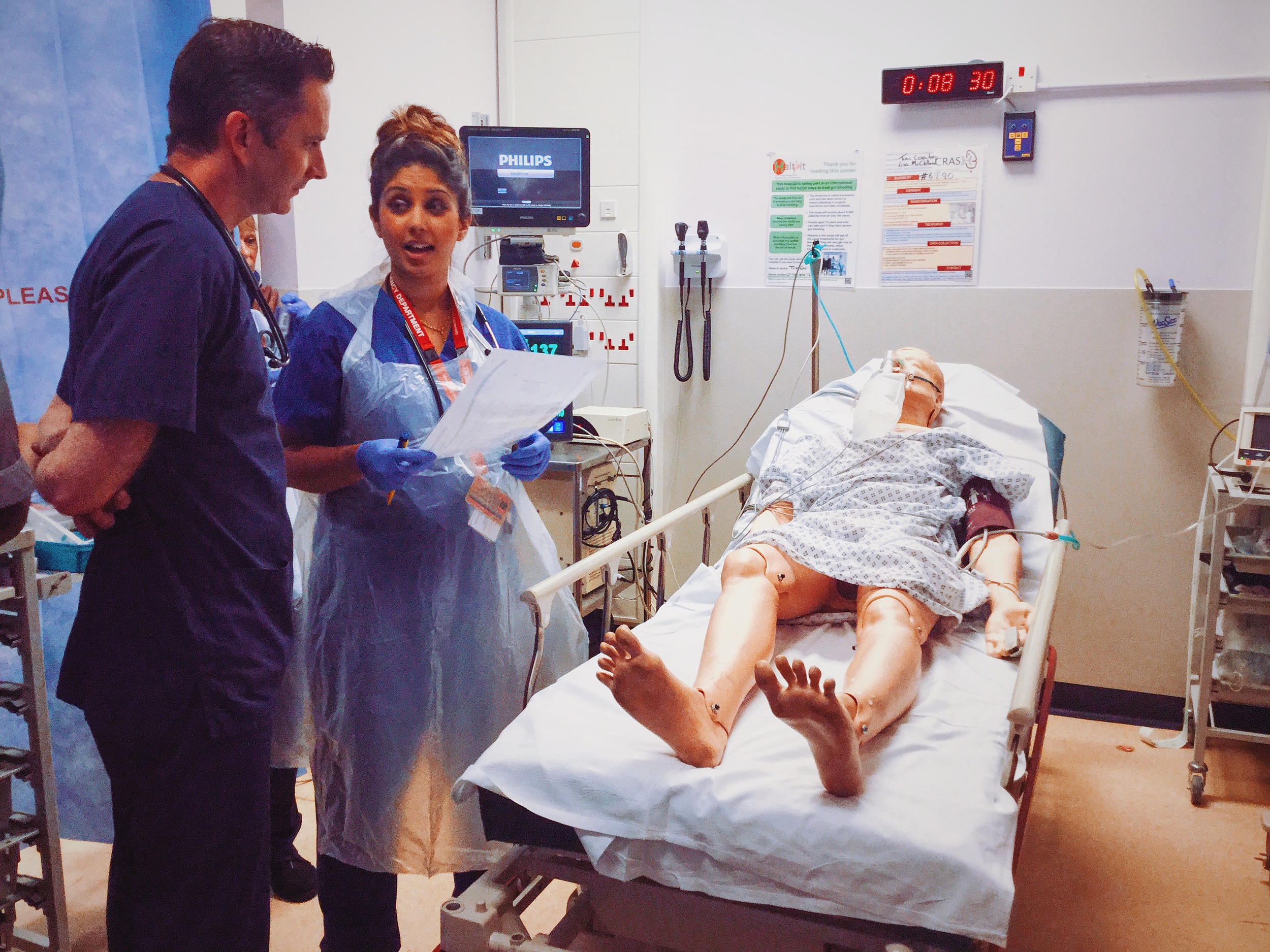
Positive Feedback
Roles Assigned
Mental Modelling
Re-assured the patient
References:
- Katharina Dworzynski, Emmert Roberts, Andrew Ludman, Jonathan Mant, 2014, Diagnosing and managing acute heart failure in adults: summary of NICE guidance British Medical Journal, 2014;349:g5695